Telemedicine and HIT are rapidly being integrated into healthcare systems around the world. These tools of ICT will become a standard of care for providing healthcare services, increasing access, decreasing unnecessary variations in care and lead to better patient and public health outcomes, locally, nationally, and internationally.
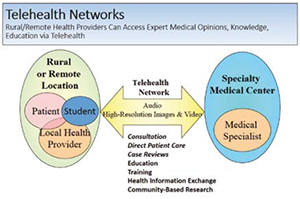
Using emerging innovations in Information and Communication Technologies (ICT), "telemedicine" is providing the tools to delivery healthcare at a distance regardless of the location of the patient and their providers, enabling access to the right care, at the right place, and at the right time.
'Telemedicine' typically refers to clinical applications of ICT, whereas 'Telehealth' reflects a broader application of ICT, including education, training, research and public health. The term such as 'eHealth' usually include the integration of electronic health records and health information exchange, and bio-medical informatics along with data analytics. South Korea uses the term 'uHealth' for ubiquitous access to healthcare. Indeed, ubiquitous wireless and cellular networks, along with the use of mobile devices; smart phones and tablets, are leapfrogging over prior barriers to healthcare delivery, leading to improved continuity of care, care that is less episodic, with the potential to improve health outcomes and prevent more serious and costly complications and avoiding the need for higher levels of care that is also more expensive.
As one travels throughout the international community, the penetration of smart phones and cellular connectivity along with internet access is clearly evident in both developing and developed countries and is dramatically changing the landscape in the global communities related to access to a wide variety of services. Specific new applications to healthcare services on mobile devices, Software as a Service (SaaS), and cloud platforms are increasing usability and adoption and also decreasing the cost. Not only are these platforms available to healthcare providers but also the consumer as a patient. Furthermore, remote monitoring devices are allowing streaming of patient data for analysis and response when appropriate.
Mobility is adding convenience for both providers and patients and dramatically changing the way in which healthcare is provided and accessed. Successful development of telehealth applications requires not only technical planning, but also operational, business, and evaluation planning that addresses defined healthcare needs. As consumers, providers of care, students, payers, and employers understand the advantages, there will increasing demand for integration of these new innovative approaches into transforming regional, national, and international healthcare systems.
As noted, the advances in mobile devices and remote monitoring are providing a new set of tools that can be utilised by healthcare providers, patients and consumers in general. Sometimes referred to as 'mHealth,' there are hundreds, if not thousands, of health related applications that can be used on smartphones and tablets, including high resolution image capture and live video conferencing. In many cases, this can avoid the purchase of more expensive end-point video conferencing equipment. However, the standards for interoperability can allow mobile devices and personal computers to communicate with stand-alone video-conferencing systems and even allow far-end camera control. When needed additional technologies applied to videoconferencing units have integrated peripheral devices to allow transmission of video or images from those devices or other cameras, such as from otoscopes, dermascopes, endoscopes and ultrasonography, as well as other devices such as electronic stethoscopes. Now these types of peripheral devices are being integrated with mobile smart phones and tablets with specialised digital 'snap-ons' placed over the mobile devices camera, such as digital microscopes, otoscopes.
Using asynchronous transmission of images called 'store and forward'; those images can be captured, stored, and forwarded, to a specialist for interpretation. For example, non-mydriatic (not requiring dilation of the pupil with medication) retinal cameras are capturing images of the retina for monitoring diabetic retinopathy or retinopathy of prematurity that can be transmitted to an eye specialist for interpretation. High resolution images of a skin abnormality can also be transmitted to a dermatologist for evaluation and management recommendations. These store and forward applications have been used for transmission of radiographic images for diagnostic interpretation by a radiologist ('teleradiology') or to augment consultations by a specialist. Similar approaches have been used in pathology ('telepathogy') for transmission of specimen or microscopic images. In addition, transmission of Electrocardiograms (ECGs) for interpretation by a cardiologist is being used. This type of store and forward technology is becoming a common application and standard within healthcare. Remote monitoring and 'wearable devices' are being developed and utilised as well, such as 'smart band aids or plasters' that can monitor vital signs, ECGs, oxygen saturation, transmit to a smart phone and into the cloud for interpretation. Due to the volume of health data, thresholds and protocols can be developed so that the appropriate healthcare providers and / or the patient or their caregivers can be alerted when monitoring data is outside normal limits. Other hand-held devices are being developed to allow the patient or their providers to measure a variety of vital signs by simply placing the device against the skin. To insure patient safety and quality of care, more regulations and guidelines are being applied to peripheral mobile or monitoring devices when used as more than a communication device. In the US, the Food and Drug Administration (FDA) has been developing regulatory standards and guidelines for the certification and use of these devices. It is anticipated that continued development of new applications, software, and devices will emerge and add to the telemedicine and HIT toolkit.
The telemedicine literature now has considerable evidence of successful utilisation of telehealth applications related to accuracy of diagnosis, patient and provider satisfaction, comparative effectiveness, cost reduction, and improved healthcare outcomes.
Telemedicine Associations have become valuable resources in navigating the telemedicine landscape, such as the 'American Telemedicine Association,' ATA that is developing standards and guidelines for the use of telemedicine, or the 'International Society for Telemedicine and eHealth, (ISFTeH) ' . The applications of ICT for healthcare have been applied in ambulatory clinics, hospital, long term care facilities, the home, schools, workplace, pharmacies and other unique settings. Telemedicine has been utilised for general health assessment and management, specialty consultation, chronic and acute disease, intensive care, mental health, and during disasters. Some of these approaches use established secure Web-based platforms for sharing patient healthcare information an images for consultations. These have included consultative support for developing countries, such as the via a system developed by the Swinfen Charitable Trust or making better triage decisions such as during patient trauma or other acute emergencies. For example, we have successfully used a secure Web-based platform that allows neurosurgeons to view brain images related to transfer requests after patient head trauma and avoided greater than 40 per cent of the transfers. In another example, applying a spectrum of ICT platforms including simultaneous multi-site video and audio conferencing, Project ECHO has used a provider education and case review model for assisting primary care providers in managing complex chronic diseases such as hepatitis C. They have demonstrated outcomes using their telemedicine approach comparable to physical face-to-face encounters and allowing access in more remote, rural settings.

Critical to the provision of virtual healthcare services via telemedicine will be the concomitant need for Health Information Exchange (HIE) using ICT. The need to have adequate health information securely shared will be part of better patient evaluation and management, as well as provide a means for addressing community and population health. Platforms are being developed and applied where individual patient information can be consolidated into one overall record from a variety of healthcare sources and different Electronic Health Records (EHRs), listing all their diagnoses, medications, allergies, immunisations, lab and radiologic data, specialist reports, patient summaries, and even images noting the time and source of that information. The HIE data can even be superimposed upon a patient's EHR allowing 'single sign on' by the healthcare provider who may prefer to work within their EHR as opposed to going to a separate portal to view the consolidated patient record. The effective use of an HIE to find a specific patient's health information requires a Master Patient Index (MPI) that can locate that patient's health information with a high degree of specificity and reasonable sensitivity inorder to avoid health information being applied to the wrong patient. An HIE also provides a means of tracking a patient's health over time and profiling their progress, as well as the achievement of a spectrum of healthcare goals. An HIE can also provide a patient portal to view their own health information in one consolidated record as opposed to going to each individual EHR's patient portal if theyare obtaining healthcare services in a variety of healthcare provider organisations using a different EHR. Determining accuracy of data will also become important with appropriate data verification monitoring and correction when needed. As larger clinical data repositories are developed, there is the opportunity to access community and population health using data analytics, determine overall health outcomes and the impact of a variety of interventions. Lastly, geospatial information systems can be applied to map health data geographically for improved situational awareness and consequence management related to both acute and chronic disease. These relational data bases superimposed upon maps can improve interpretation of the health data and allow more effective and appropriate interventions and utilisation of resources.
The functionality of these telemedicine applications is dependent upon an adequately trained workforce in both the healthcare and ICT domains. As these systems become more widely used, attention to having local ICT support becomes more critical, as well as having adequately trained health professionals to effectively utilise these new telemedicine platforms. In many areas of the developing world, providing training and development of healthcare professionals will be a critical part of the having a robust healthcare system. These ICT technologies can also provide a 'virtual' classroom for training, education, and sharing knowledge of healthcare students and providers, as well as IT students and professionals. Furthermore, these telemedicine and HIE systems will need to be integrated into operational workflow in order to promote adoption and meaningful use. Approaches to ensuring adequately trained healthcare professionals with verified credentials and qualifications will also become increasingly important as these systems penetrate into the global market and healthcare services are provided internationally. Technologies to authenticate the identity of the virtual provider will also become important in ensuring quality of care and avoidance of abuse. Training in the effective use of these systems for patients and consumers needs to be addressed as the consumer becomes a major participant in maintaining their health, and the concept of the patient-centered medical home is promoted. By working collaboratively in the international environment, telemedicine, HIE, and HIT can be developed in a manner that is culturally appropriate, and meets healthcare needs based on resources available in each country, addressing the health of people throughout the world.

ACOs promote collaborative care and tie provider reimbursements to quality metrics and reductions in cost of care for an assigned population of patients. ACOs are increasingly promoting value-based pricing models such as bundled payments, risk based capitation and thereby helping payers to share financial risk with providers. Collaborative care in healthcare is also being driven by the ARRA Act and meaningful use clauses among providers. Providers are now focusing on technological capabilities to share data with use of Electronic Health Records (EHRs) and Health Information Exchange networks (HIEs) and perform predictive modeling while delivering care services.
In order to adequately support telemedicine and HIE applications, there is an increasing need and demand for adequate, affordable broadband connectivity. Some high-speed internet fiber backbones are being integrated with healthcare applications, such as Internet2 and National Lambda Rail. More wireless connectivity is also being utilised via satellite, microwave, and cellular networks. Cellular networks are becoming more ubiquitous globally having a significant impact in developing countries as they bring access to healthcare services and information not previously available. As healthcare systems become more dependent upon telemedicine and HIE, there will also be a need for increasing network reliability and disaster recovery with backup power supply and redundant connectivity pathways if one component of the networks become inoperable. There will be an increasing need for network operating services to continually monitor and provide rapid detection and correction of network problems. The challenge of deploying and managing adequate and affordable broadband in the most rural and remote areas of the world needs to be addressed by individual counties and telecommunication service providers
Telemedicine and HIT are rapidly being integrated into healthcare systems around the world. These tools of ICT will become a standard of care for providing healthcare services, increasing access, decreasing unnecessary variations in care and lead to better patient and public health outcomes, locally, nationally, and internationally. When applied effectively, they also hold the promise of decreasing healthcare costs. Furthermore, through these ICT systems can enable mutual international healthcare collaboration and cultural understanding through the sharing of health-related knowledge and experience that is just in time, on demand, and provide evidence-based best practices relevant to the populations served. In the future 'telemedicine' and HIT should no longer be viewed as separate approaches to healthcare but become fully adopted and integrated into healthcare delivery systems around the world, providing the right care, at the right place, at the right time.